ICD-10 code E03.9 is widely used in outpatient and inpatient settings because hypothyroidism is common, chronic, and often managed across primary care and specialties. But “unspecified” coding can create downstream friction when documentation is thin—especially when claims need a clear diagnosis-to-service connection for medical necessity (labs, follow-ups, medication management). The good news: most E03.9 problems are preventable with a consistent provider note structure and a coder workflow that validates specificity in the ICD-10-CM tabular list and official guidelines. This guide explains what E03.9 means, when to use it (and when not to), and how to document and code it cleanly.
ICD-10 code E03.9 means hypothyroidism, unspecified in ICD-10-CM. Use it when the provider documents hypothyroidism but does not specify the type or cause in the assessment for that encounter. If documentation supports a more specific hypothyroidism diagnosis (e.g., congenital, postprocedural, drug-induced), code to that specificity. Verify in ICD-10-CM tabular list + official guidelines.
What Does ICD-10-CM Code E03.9 Mean?
E03.9 is the ICD-10-CM diagnosis code for “Hypothyroidism, unspecified.” It’s a billable code used when hypothyroidism is documented but the record does not specify a more precise hypothyroidism category.
What “unspecified” means (plain language)
“Unspecified” does not mean “uncertain” or “rule-out.” It means the provider documented hypothyroidism, but did not document enough detail to assign a more specific ICD-10-CM code. In practice, E03.9 often appears when:
- hypothyroidism is carried as a chronic problem but etiology isn’t stated, or
- the visit focuses on monitoring labs/med refills without clarifying type.
Coding best practice is to use the highest specificity supported by documentation and the full number of characters required by ICD-10-CM.
When to Use E03.9 (and When NOT To)
Use E03.9 when the provider’s final assessment documents hypothyroidism but doesn’t specify the type/cause. Don’t use E03.9 if the record supports a more specific hypothyroidism code—coders should validate in the tabular list and follow official guidelines.
Appropriate scenarios (E03.9 is reasonable)
- Provider documents “hypothyroidism” in the Assessment/Problem List with no additional detail on etiology/type.
- The encounter is routine management (e.g., medication monitoring, stable disease follow-up) and the record does not specify postprocedural, congenital, drug-induced, etc.
- The documentation supports hypothyroidism as a current condition being addressed (not merely a historical mention).
When NOT to use E03.9 (documentation supports more specificity)
- Provider documents a specific type/cause (e.g., congenital hypothyroidism, postprocedural hypothyroidism, drug-induced hypothyroidism, iodine deficiency-related hypothyroidism).
- The record clearly indicates a different thyroid disorder category (e.g., thyroiditis-related conditions) that is coded elsewhere.
- The diagnosis is not confirmed (e.g., “rule out hypothyroidism,” “possible hypothyroidism”) in outpatient settings—follow the official guideline approach for uncertain diagnoses in outpatient coding and code what is documented as established/treated.
Rule of thumb: If the provider gives you the “why,” you should usually be coding more specifically than E03.9—after confirming in the ICD-10-CM tabular list.
Documentation Checklist for Clean Coding
Clean coding for E03.9 starts with a clear provider diagnosis statement and clinical context. You don’t need a long note, but you do need enough detail to support diagnosis coding and medical necessity for services like labs and follow-up visits.
Use this documentation checklist (8–12 items):
- Diagnosis statement: “Hypothyroidism” documented in Assessment (not just in lab review).
- Type/etiology if known: primary vs secondary/central, postprocedural, drug-induced, congenital, etc. (only if established and documented).
- Chronicity/status: new diagnosis vs chronic/stable vs uncontrolled/undertreated (clinical wording).
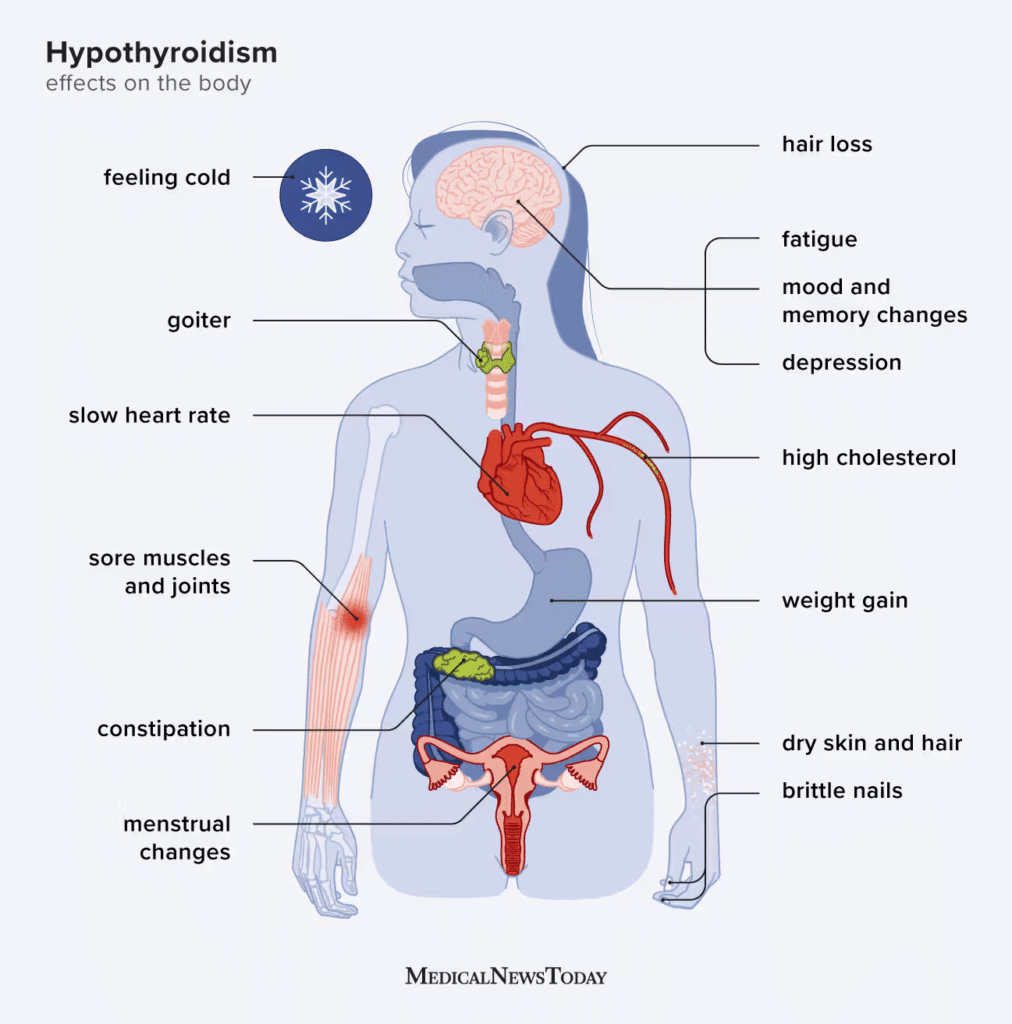
- Relevant symptoms when addressed (e.g., fatigue, cold intolerance)—avoid copying templates without clinical relevance.
- TSH value and trend (e.g., elevated, improving, worsening) and date of lab.
- Free T4 (and other labs if used) and date—especially if it changes management.
- Treatment status: thyroid hormone replacement (e.g., levothyroxine) documented as continuing, adjusted, started, or held.
- Medication details impacting care: dose change rationale, adherence issues, interactions (only when assessed).
- Comorbidities affecting management (e.g., pregnancy status, cardiac disease) if evaluated and relevant.
- Plan of care: follow-up interval, repeat lab timing, and medication monitoring plan.
Why this matters: ICD-10-CM guidance emphasizes coding to the highest level of specificity supported by the medical record.
E03.9 vs Other Hypothyroidism Codes (How to Choose)
Coders choose between E03.9 and other hypothyroidism codes by following the Index → Tabular List → guidelines workflow and coding to the highest specificity documented. ICD-10-CM rules require using the full code length and the most specific code supported.
A practical “how to choose” workflow
- Start with provider documentation (Assessment/diagnosis statement and plan).
- Look up the main term (hypothyroidism) in the ICD-10-CM Index.
- Validate in the Tabular List:
- confirm the correct category and code title,
- check instructional notes (includes/excludes),
- confirm code completeness.
- Apply official ICD-10-CM guidelines (highest specificity supported; outpatient uncertain diagnoses guidance; etc.).
- If documentation is unclear, query the provider (brief, specific question: “Is this postprocedural? drug-induced? central?”).
3–5 common mistakes to avoid
- Mistake 1: Defaulting to E03.9 when the note states a specific etiology. If the provider documents a cause/type, you should usually select a more specific hypothyroidism code (after tabular verification).
- Mistake 2: Coding from labs alone. An abnormal TSH supports the diagnosis but doesn’t replace a provider diagnosis statement for that encounter.
- Mistake 3: Treating “unspecified” as a catch-all for uncertainty. “Unspecified” ≠ “rule out.” In outpatient settings, uncertain diagnoses should not be coded as established diagnoses.
- Mistake 4: Not coding to full specificity/characters. ICD-10-CM requires full characters and highest specificity when supported.
- Mistake 5: Forgetting medical necessity linkage. If you’re billing thyroid labs or medication management, the note should connect hypothyroidism management to the ordered services.
Billing & Denial Risks (How E03.9 Affects Claims)
E03.9 can be claim-safe, but it may increase friction when payers expect clearer specificity or stronger medical necessity documentation for related services. Denials aren’t guaranteed—many claims pay with E03.9—but “thin” documentation can raise audit/records-request risk and slow reimbursement.
Common billing/edit issues to watch:
- Medical necessity narratives for labs: If TSH/free T4 testing is billed, documentation should show hypothyroidism management and monitoring rationale (especially when frequency is higher than typical).
- Problem-list-only diagnosis: A claim may be challenged if hypothyroidism is listed historically but not addressed in the assessment/plan for the DOS.
- Unclear status/treatment: If thyroid hormone replacement is managed, note the status (stable vs dose change) and lab plan.
- Comorbidity-driven complexity not captured: If comorbidities materially affect management and are documented/treated, ensure they’re coded appropriately (don’t add diagnoses that aren’t supported by the note).
Denial prevention tips (non-payer-specific):
- Ensure hypothyroidism is explicitly assessed and tied to orders (labs, med refills).
- Use a consistent template that prompts etiology/type when known (postprocedural, drug-induced, etc.).
- If E03.9 is used frequently, run periodic audits and provider education focused on “what detail changes the code.”
(If you’re unsure whether a more specific code is required, verify in ICD-10-CM tabular list + official guidelines.)
Best Practices for Clinics & Hospitals
The fastest way to improve E03.9 accuracy is to align provider documentation prompts with coder decision points. This reduces coder queries, improves specificity, and supports cleaner claims.
Quick wins:
- EHR templates: Add prompts in endocrine/primary care notes for “type/etiology” (if known), current treatment, and lab plan.
- Coder query process: Use short, closed-ended queries (e.g., “Is hypothyroidism postprocedural?” “Drug-induced?” “Central?”) when documentation suggests it.
- Internal audits: Review a small sample of hypothyroidism claims monthly—focus on E03.9 frequency, missing specificity opportunities, and documentation gaps.
- Coder-provider alignment: Share examples of what documentation changes coding (and why), emphasizing the guideline principle: code to the highest specificity supported.
- Medical necessity support: Ensure TSH/free T4 orders are linked to assessment and plan, not just copied forward.
FAQs
What is ICD-10 code E03.9?
ICD-10 code E03.9 is the ICD-10-CM code for hypothyroidism, unspecified. It’s used when the provider documents hypothyroidism but doesn’t specify a more detailed type/cause.
What does “unspecified hypothyroidism” mean?
It means hypothyroidism is documented, but the record lacks enough detail to code a more specific hypothyroidism category. “Unspecified” is about missing specificity, not necessarily clinical uncertainty.
When should E03.9 be used?
Use E03.9 when hypothyroidism is a confirmed provider diagnosis for the encounter and no additional specificity (etiology/type) is documented. If documentation supports specificity, code that instead—verify in ICD-10-CM tabular list and guidelines.
Can E03.9 cause claim denials?
It can contribute to denials or records requests when documentation doesn’t support medical necessity for related services (like lab frequency) or when payers expect clearer specificity. Many claims still process—but good documentation reduces friction.
How can providers document hypothyroidism for accurate coding?
Include an assessment diagnosis statement, relevant labs (TSH/free T4 with dates/trends), treatment status (thyroid hormone replacement), and etiology/type when known (postprocedural, drug-induced, etc.). Tie orders to the plan.
Is E03.9 okay for chronic/stable hypothyroidism?
Often yes—if the provider documents hypothyroidism as an active condition being managed during that visit. If the chart supports a more specific hypothyroidism type, use the more specific code after tabular verification.
Do coders need TSH to code E03.9?
TSH supports the clinical picture, but coding is documentation-driven: the provider’s diagnosis statement and assessment/plan determine whether hypothyroidism is coded for that encounter.
What if the provider documents the cause—should I still use E03.9?
Usually no. If a cause/type is documented and supported, coders should select the most specific hypothyroidism code available and confirm it in the ICD-10-CM tabular list and official guidelines.
Conclusion
ICD-10 code E03.9 works when hypothyroidism is documented but not specified. To reduce denials and rework, document the diagnosis in the assessment, include key labs (TSH/free T4), note thyroid hormone replacement status, and specify the cause when known—then code to the highest specificity and verify in the ICD-10-CM tabular list and official guidelines.

